Springbuk launches partner marketplace for employers and benefits advisors
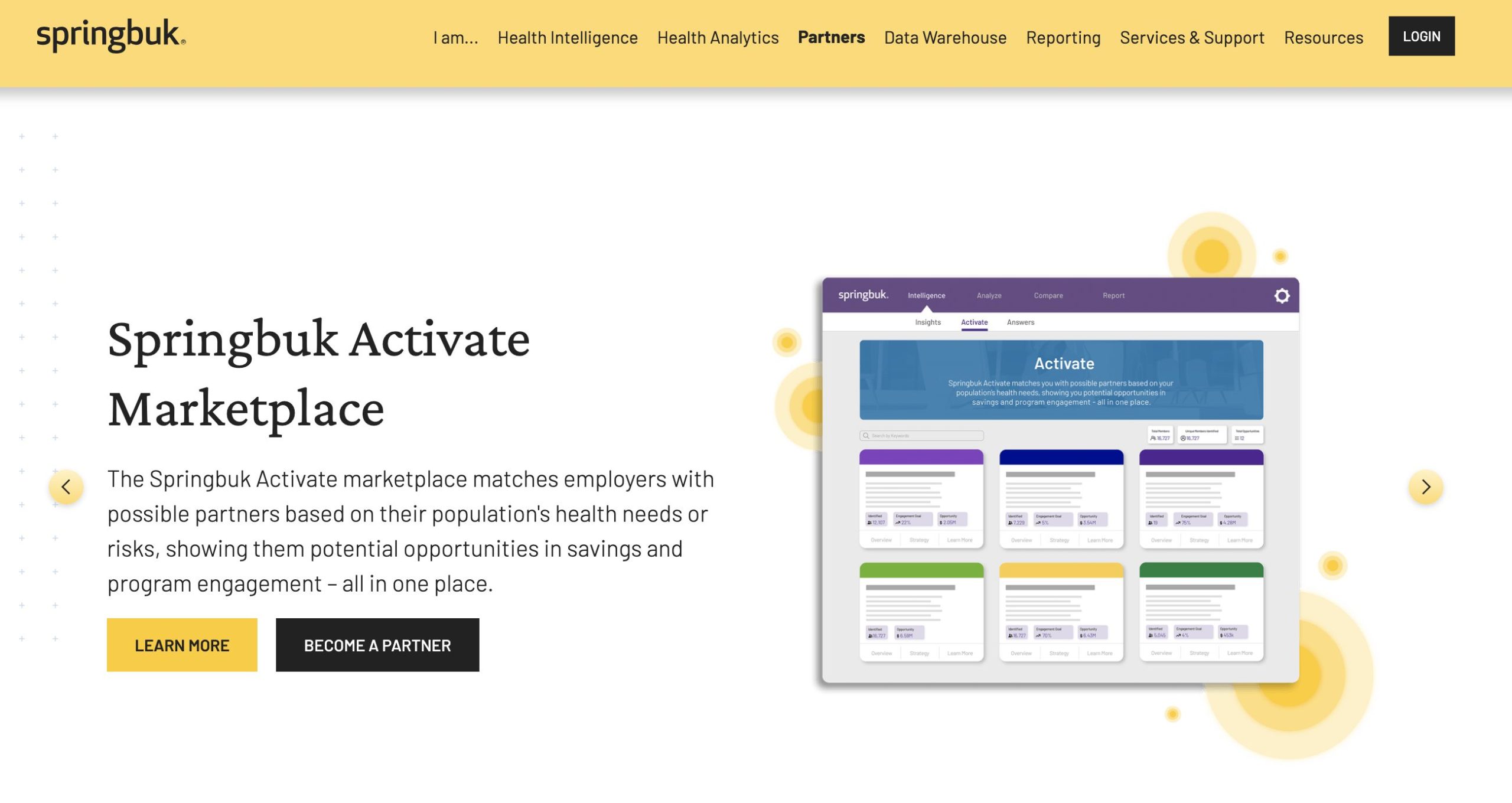
Health intelligence and analytics platform Springbuk announced the general availability of a new partner marketplace within the Springbuk Health Intelligence™ platform. The Springbuk Activate marketplace matches employers with possible partners based on their population’s health needs or risks, showing them potential opportunities in savings and program engagement.
Eleven partners were announced in this inaugural rollout with more expected to join in phases throughout the first quarter and the remainder of 2024. The initial set of partners is:
- HealthJoy – Guiding employees to affordable, high-quality care to improve health outcomes and contain costs.
- Hinge Health – The musculoskeletal leader in digital MSK care, transforming the way pain is treated and prevented.
- Included Health – Expert Medical Opinion provides guidance from leading experts to improve care outcomes for members with complex conditions.
- Jellyvision – ALEX by Jellyvision helps employees confidently understand and choose the right benefits, without breaking the bank.
- Noom – A full-spectrum metabolic health solution that combines biological and psychological support for lasting health outcomes.
- PHM ClearCancer™ – expert cancer care management to achieve the best of what’s possible in medicine.
- Renalogic – Comprehensive management of kidney disease and dialysis, effectively containing costs and improving patient outcomes.
- Reperio – Only provider of at-home & onsite biometric screenings with instant results, enabling convenient access to preventive care.
- RxBenefits – Optimizing pharmacy benefits for employers to achieve lowest net cost and mitigate risk without sacrificing service.
- Summus – A leading virtual health company, accelerating access to specialty expertise, providing guidance, education, and advocacy.
- Transcarent – the one place for health and care, makes it easy for people to access high-quality, affordable care.
“The Springbuk Activate marketplace represents a seismic shift in how employers and their benefits advisors can now plan and execute their benefits programs. Springbuk has always excelled at identifying opportunities for population health management, risk management, and cost containment. Now we’re taking the next step – delivering a data-driven program, using the employers’ underlying data, to uniquely match the employer population needs with a partner program. We are proud to join forces with these organizations, each of which brings unique strengths to our platform. Together, we are pioneering a new era in health management, where data-driven insights meet individualized care.” – Joy Powell, Springbuk CEO.
Springbuk worked with each partner featured in the Activate marketplace to fully customize a “card” within the Springbuk application that displays the partner’s logo, program description, value proposition, and strategy for realizing opportunities. The identified members and corresponding savings opportunity displayed in the Springbuk application are generated by each partner’s proprietary methods or calculations. Springbuk then applies the methodology on the underlying employer data.
For an employer or benefits advisor, Springbuk Activate provides an estimate of:
- The number of members in the employer’s population who may qualify for a partner’s program
- An estimated engagement rate for the partner’s program, which represents the percentage of the members identified who are likely to engage in the partner’s program
- An annual (12-month) savings opportunity estimate based on the partner’s assumptions of program success

