Shift Technology partners with Cigna
Shift Technology, a provider of AI-native fraud detection and claims automation solutions, is partnering with Cigna to strengthen its fraud detection capabilities within the claims process. As part of the partnership, Cigna will evaluate Shift’s fraud detection solution ‘Force’ to support its International Operations Unit, which designs, implements and manages international group health insurance and employee benefits programs for globally mobile employees.
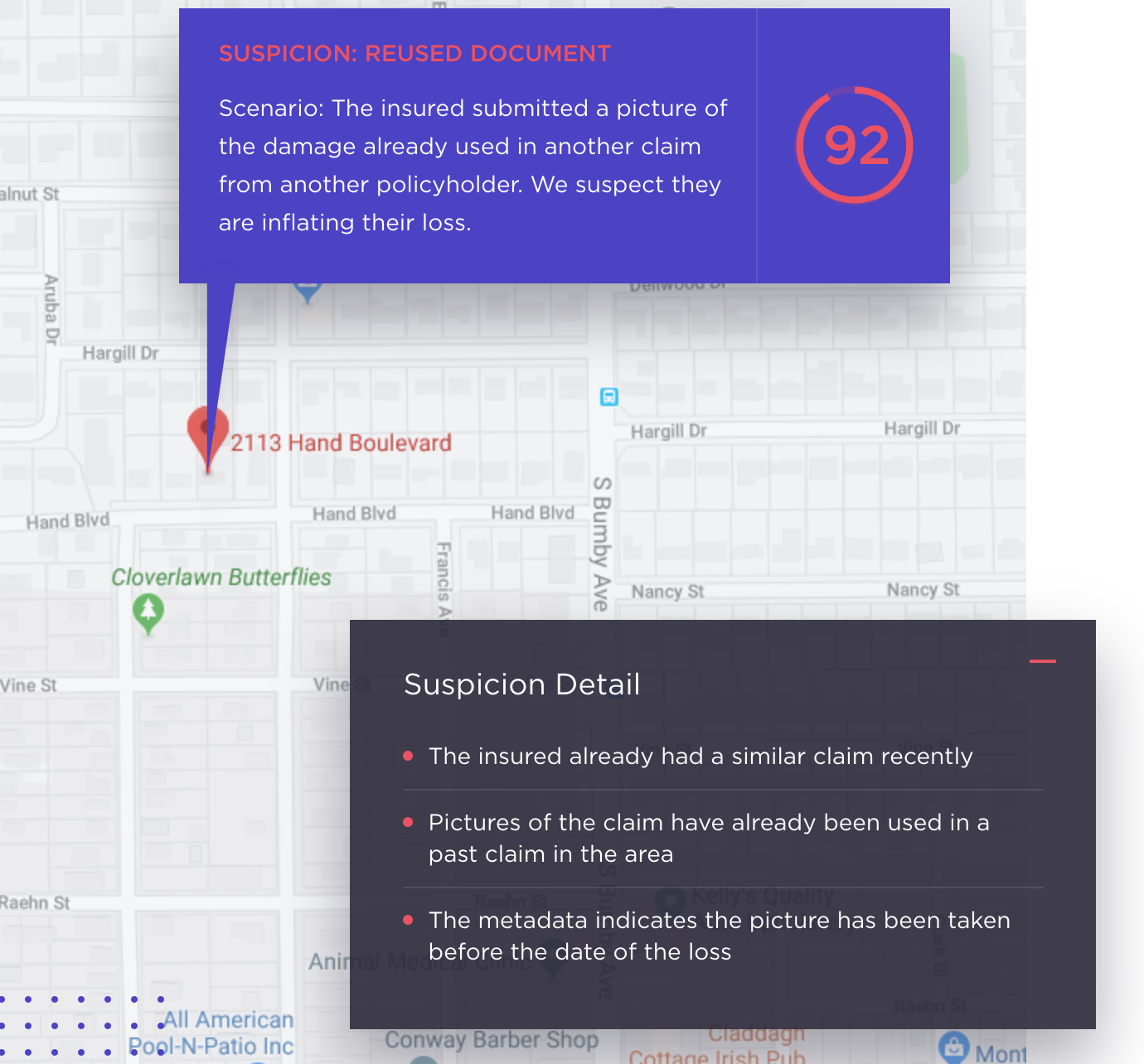
Shift’s Force can tighten the level of security by identifying potential fraud perpetrated by individuals. The product enhances security by making correlations within the insurer’s full data set, allowing the technology to build and connect the “social networks” of related entities to detect and extract only the most highly suspicious “sub-networks” within the larger networks.
“Applying Force’s AI-native technology to the health insurance claims process significantly increases the discovery of fraud, waste and abuse cases before the claim is paid. This is incredibly important – it gives Cigna the power to fight fraud proactively rather than ‘after the fact’ when payments for illegitimate claims may have already been made.” – Jeremy Jawish, CEO and cofounder, Shift Technology.
“Fraud is not a ‘victimless’ crime, and it’s not only insurers that could be hurt by it. Everyone, especially policyholders, lose when fraud goes undetected and non-meritorious claims are paid. We’ve long taken a holistic approach to fighting fraud and continuously look for innovative ways to improve our capabilities in fraud detection. Identifying suspicious claims earlier and better understanding why they were flagged, means we can act even quicker to investigate and reach the best possible resolution for our customers and clients.” – David Curlett, Head of Fraud Waste and Abuse at Cigna.





